Sleep is essential for physical health, emotional well-being, cognitive functioning, and overall quality of life. When sleep becomes disrupted—whether from snoring, frequent awakenings, or daytime fatigue—it may signal an underlying sleep disorder. That’s where a sleep study, also known as a polysomnogram, comes in. It’s a powerful diagnostic tool used by sleep specialists to understand what’s going on in the body during sleep and to guide effective treatment.
In this article, we will explore the process of a sleep study in detail: what it is, who it’s for, what it involves, and what to expect before, during, and after the study.
What is a Sleep Study?
A sleep study is a comprehensive overnight evaluation that records your brain waves, blood oxygen levels, heart rate, breathing, and eye and leg movements while you sleep. The goal is to assess how well you sleep and identify any disturbances that may point to conditions such as:
- Obstructive Sleep Apnea (OSA)
- Central Sleep Apnea
- Periodic Limb Movement Disorder (PLMD)
- Narcolepsy
- Insomnia
- REM Behavior Disorder
- Restless Leg Syndrome
Sleep studies are usually conducted in a sleep center or hospital, though some can be done at home with portable monitoring equipment.
Types of Sleep Studies
There are several types of sleep studies, and the right one depends on your symptoms and clinical history:
- In-Lab Polysomnography (PSG):
This is the most comprehensive type and is conducted in a specialized sleep laboratory. It’s used to diagnose complex cases or when high-quality data is necessary. - Home Sleep Apnea Test (HSAT):
For patients with a high likelihood of moderate to severe obstructive sleep apnea, a simpler version can be conducted at home using a portable device. It typically measures breathing, oxygen levels, and heart rate—but does not record brain waves. - Multiple Sleep Latency Test (MSLT):
This daytime test evaluates how quickly you fall asleep in a quiet environment and how quickly you enter REM sleep. It’s primarily used to diagnose narcolepsy. - Maintenance of Wakefulness Test (MWT):
This test evaluates how well you can stay awake during the day, often used in safety-critical professions or in assessing the effectiveness of treatment.
Who Should Consider a Sleep Study?
Sleep studies are recommended for individuals experiencing the following symptoms:
- Loud snoring with pauses in breathing
- Daytime sleepiness or fatigue
- Frequent nighttime awakenings or insomnia
- Gasping or choking during sleep
- Morning headaches
- Mood changes or difficulty concentrating
- Unexplained high blood pressure
- Abnormal movements during sleep
- Sudden sleep attacks during the day
What Happens Before the Sleep Study?
1. Clinical Evaluation:
Your sleep specialist will review your medical history, symptoms, and medications. They may use questionnaires such as the Epworth Sleepiness Scale or STOP-BANG to assess your risk for conditions like sleep apnea.
2. Preparation Guidelines:
You’ll receive specific instructions on how to prepare for the study. Typically, you’ll be asked to:
- Avoid caffeine and alcohol on the day of the test
- Wash your hair (no oils or products)
- Bring comfortable sleepwear and personal items
- Continue taking medications unless instructed otherwise
If it’s a home sleep study, you’ll be given training on how to apply the device properly.
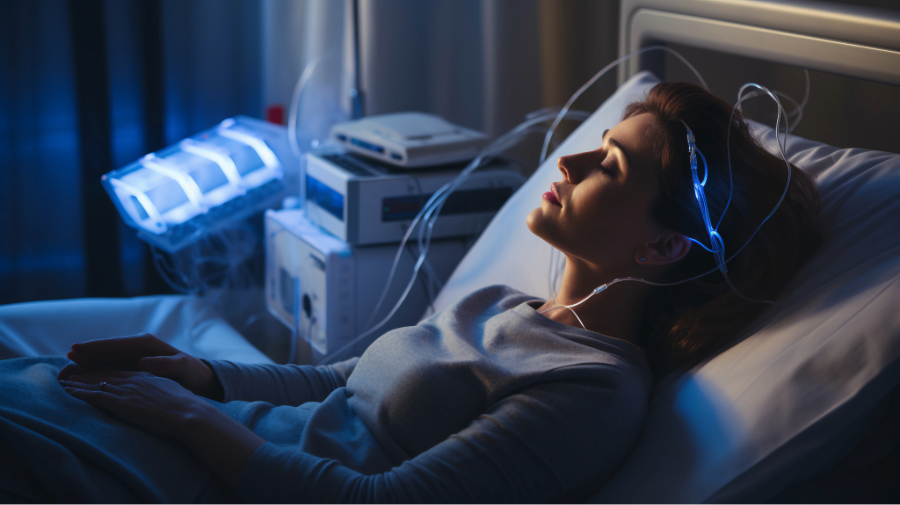
What to Expect During an In-Lab Sleep Study
An in-lab study usually starts in the evening and lasts until early morning.
1. Arrival and Setup:
You’ll check in at the sleep center in the evening, usually between 8 and 9 PM. A sleep technologist will greet you and help you settle into a private room that resembles a hotel room more than a hospital.
2. Hooking Up Sensors:
The technologist will apply sensors to your scalp, face, chest, abdomen, legs, and fingers using paste or adhesive pads. These sensors monitor:
- EEG (Electroencephalogram): Brain wave activity
- EOG (Electrooculogram): Eye movements
- EMG (Electromyogram): Muscle tone in the chin and legs
- ECG (Electrocardiogram): Heart rate and rhythm
- Respiratory channels: Airflow through the nose/mouth, chest and abdominal movement
- Pulse oximetry: Blood oxygen saturation
You’ll still be able to move, roll over, and sleep in your normal positions. A microphone records snoring, and a camera records movements for video analysis.
3. Overnight Monitoring:
Once you’re ready to sleep, the technologist will monitor you from a control room. If any equipment needs adjustment during the night, they may briefly enter the room.
If you’re undergoing a CPAP titration (for known sleep apnea), a mask will be fitted and adjusted throughout the night to determine the optimal pressure needed to prevent airway collapse.
What Happens After the Sleep Study?
1. Morning Disconnection:
You’ll typically be woken around 6–7 AM. The sensors are removed, and you’ll be free to go home or to work.
2. Data Analysis:
The recorded data is scored manually by a technologist and then reviewed by your sleep specialist. The report will analyze:
- Sleep stages and architecture (REM, NREM)
- Total sleep time and sleep efficiency
- Respiratory events (apneas, hypopneas)
- Arousal index
- Oxygen desaturation events
- Limb movements
3. Diagnosis and Treatment Plan:
Your doctor will review the results with you in a follow-up appointment, usually within 1–2 weeks. Depending on the diagnosis, treatment options may include:
- CPAP (Continuous Positive Airway Pressure): For sleep apnea
- Oral appliances: For mild to moderate OSA
- Behavioral therapy: For insomnia or circadian rhythm disorders
- Medication: For narcolepsy or restless leg syndrome
- Lifestyle modifications: Weight loss, sleep hygiene, avoiding alcohol
Common Concerns and Misconceptions
“I won’t be able to sleep with all those wires.”
This is a common concern, but most patients sleep better than they expect. Even with reduced sleep time, we typically gather enough data to make an accurate diagnosis.
“Is it uncomfortable or painful?”
The test is non-invasive and painless. The sensors may feel unusual at first, but they don’t hurt.
“Why can’t I just do a home test?”
Home sleep apnea tests are convenient and cost-effective, but they’re not appropriate for everyone. They don’t record brain activity or leg movements, and they may miss certain sleep disorders. Your doctor will decide which test is best for your situation.
Final Thoughts
A sleep study is an invaluable diagnostic tool in modern medicine. It offers a window into your body’s functioning during sleep and can reveal disorders that are silently affecting your health, mood, and quality of life. Whether performed in a lab or at home, the information gathered can lead to effective treatment strategies that help you sleep better—and live better.
If you’re struggling with poor sleep, excessive daytime fatigue, or any unusual nighttime symptoms, don’t wait. Speak with a board-certified sleep specialist and find out if a sleep study is the right next step. Restful, restorative sleep may be closer than you think
Are you interested in a sleep study, if so, please call Sweet Sleep Studio at (913) 309-5963.