Sleep is essential for good health, yet millions of people suffer from sleep disorders that can significantly impair their quality of life. One of the most common—and potentially dangerous—sleep disorders is Obstructive Sleep Apnea (OSA). As a medical sleep specialist, I aim to shed light on what OSA is, its causes, symptoms, diagnostic procedures, and treatment options to help patients and families recognize and properly manage this condition.
What Is Obstructive Sleep Apnea?
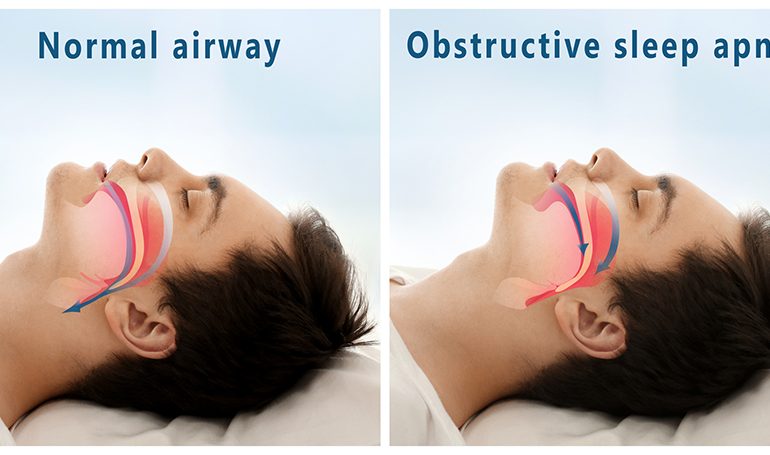
Obstructive sleep apnea is a disorder in which breathing repeatedly stops and starts during sleep due to a physical blockage in the upper airway. Unlike central sleep apnea, which involves the brain failing to send the correct signals to the muscles that control breathing, OSA is mechanical in nature. The soft tissues at the back of the throat—like the tongue, uvula, soft palate, or tonsils—can relax excessively and collapse, blocking the airway and making it difficult or impossible to breathe.
When this happens, the body is jolted out of deep sleep to resume breathing—often without the person being fully aware of the disturbance. These repeated arousals lead to fragmented, poor-quality sleep and can cause a host of health problems if left untreated.
Who Is at Risk?
Obstructive sleep apnea can affect anyone, including children, but certain factors increase the risk:
- Excess weight: Obesity is one of the most significant risk factors for OSA. Fat deposits around the upper airway can obstruct breathing.
- Neck circumference: People with thicker necks may have narrower airways, increasing the chance of blockage.
- Narrow airway: Some people naturally have a narrower throat or enlarged tonsils/adenoids.
- Male gender: Men are more likely to develop OSA than women, although the risk for women increases after menopause.
- Age: OSA is more common in older adults.
- Family history: Genetics can play a role.
- Use of sedatives or alcohol: These substances relax throat muscles, increasing the likelihood of airway obstruction.
- Smoking: Smoking increases inflammation and fluid retention in the upper airway.
Signs and Symptoms
Because obstructive sleep apnea occurs during sleep, many people are unaware they have it. Often, it’s a bed partner who first notices the warning signs. Common symptoms include:
- Loud, chronic snoring
- Episodes of breathing cessation observed by another person
- Gasping or choking during sleep
- Excessive daytime sleepiness
- Morning headaches
- Difficulty concentrating or memory problems
- Irritability or mood changes
- Waking up with a dry mouth or sore throat
- Frequent nighttime urination (nocturia)
Children with OSA may exhibit symptoms such as bedwetting, behavioral problems, hyperactivity, and poor school performance.
Health Consequences of Untreated OSA
Untreated obstructive sleep apnea goes beyond daytime fatigue. It can lead to serious, even life-threatening complications, including:
- High blood pressure
- Heart disease (e.g., arrhythmias, heart attack, heart failure)
- Stroke
- Type 2 diabetes
- Metabolic syndrome
- Depression and anxiety
- Cognitive impairment
- Increased risk of accidents (e.g., drowsy driving)
OSA has also been linked to poorer outcomes in surgery and anesthesia, making early diagnosis and treatment essential.
Diagnosing Obstructive Sleep Apnea
Diagnosis of OSA begins with a comprehensive sleep evaluation, which may include a detailed medical history, physical exam, and sleep questionnaires. If OSA is suspected, the gold standard for diagnosis is a sleep study, formally known as polysomnography.
There are two main types of sleep studies:
- In-lab polysomnography: Conducted overnight in a sleep center, this test monitors brain waves, oxygen levels, heart rate, breathing, and movements.
- Home sleep apnea test (HSAT): A simplified version done at home for patients with high likelihood of moderate to severe OSA. It measures airflow, breathing patterns, oxygen levels, and sometimes heart rate.
The sleep study provides an Apnea-Hypopnea Index (AHI)—a number that indicates how many apneas and hypopneas occur per hour of sleep:
- Mild OSA: 5–14 events/hour
- Moderate OSA: 15–29 events/hour
- Severe OSA: 30+ events/hour
Treatment Options
Fortunately, OSA is highly treatable. The appropriate therapy depends on the severity of the condition and the patient’s individual needs.
1. Lifestyle Modifications
- Weight loss: Even a modest weight reduction can significantly improve symptoms.
- Positional therapy: Some people only experience OSA when sleeping on their back. Special pillows or alarms can help keep them sleeping on their side.
- Avoid alcohol and sedatives: These relax airway muscles and worsen OSA.
- Quit smoking: Reduces airway inflammation and fluid retention.
2. Continuous Positive Airway Pressure (CPAP)
CPAP is the most effective and commonly prescribed treatment for moderate to severe OSA. It delivers a steady stream of air through a mask to keep the airway open during sleep. When used consistently, CPAP improves sleep quality, reduces daytime sleepiness, and lowers cardiovascular risk.
3. Oral Appliance Therapy
For patients with mild to moderate OSA or those who cannot tolerate CPAP, a dentist trained in sleep medicine can fit an oral appliance. These devices reposition the lower jaw or tongue to keep the airway open.
4. Surgery
Surgical options may be considered when other treatments fail. Procedures include:
- Uvulopalatopharyngoplasty (UPPP): Removes excess tissue from the throat.
- Genioglossus advancement: Repositions tongue muscles.
- Maxillomandibular advancement: Moves the jaw forward to enlarge the airway.
- Inspire therapy (hypoglossal nerve stimulation): A newer, implantable device that stimulates throat muscles to keep the airway open during sleep.
5. Treatment of Related Conditions
For patients with nasal congestion or enlarged tonsils, addressing those issues—such as through allergy management or tonsillectomy—can improve airway patency.
Living with OSA: Long-Term Management
Managing obstructive sleep apnea is often a lifelong commitment. Patients should continue regular follow-ups with a sleep specialist to monitor progress, adjust therapies, and address new or changing symptoms.
Consistent use of prescribed treatments—especially CPAP—can dramatically improve not only sleep but overall health, energy, mood, and quality of life. With proper management, patients can live full and active lives without the dangerous complications associated with untreated OSA.
Conclusion
Obstructive sleep apnea is a common but underdiagnosed disorder that can have serious consequences if left untreated. Fortunately, with increased awareness, proper diagnosis, and individualized treatment, most patients experience significant improvement in both sleep and overall health. If you or someone you love snores loudly, feels excessively tired during the day, or has observed breathing pauses during sleep, don’t ignore the signs—speak to a medical sleep specialist and take the first step toward better rest and better health.
If you’re experiencing Obstructive Sleep Apnea, please call Sweet Sleep Studio at (913) 309-5963.